How to Avoid Athlete Burnout and Overtraining Syndrome this Winter

Winter can be a challenging time of year for many athletes. However, the offseason and the preseason can be long and grueling. Without the thrill of competition, it may seem impossible to avoid what many athletes refer to as staleness, burnout, chronic fatigue syndrome, or what clinicians define as overtraining syndrome (OTS).1 Discover what overtraining syndrome is and how to avoid it in order to maximize athlete performance.
Definition: Overtraining syndrome is best defined using a spectrum (see Figure 1). Training usually entails an overload that is used to disturb homeostasis, resulting in acute fatigue leading to an improvement in athlete performance. When training continues or when athletes use a short time frame (e.g. training camp) they can experience a brief performance decrement with an eventual improvement in performance and recovery. When athletes do not sufficiently respect the balance between training and recovery, extreme overreaching can occur. If there is prolonged maladaptation with clinical, hormonal, and other signs discussed below, overtraining syndrome can occur.1,2,3
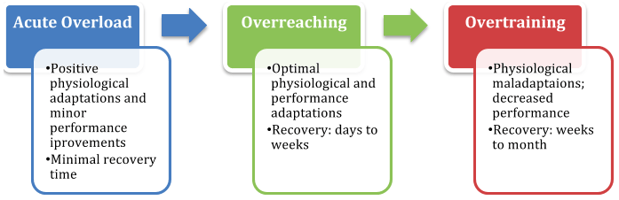
Figure 1
Signs of Overtraining
The initial symptom of OTS is usually fatigue and unexplained underperformance. In time, the symptoms displayed in Figure 2 may develop.5,6
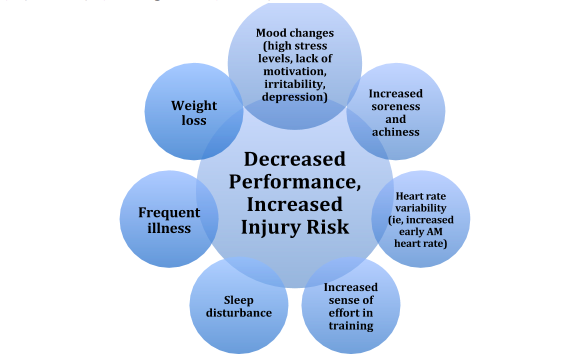
Figure 2
Prevention of Overtraining
- Use a training log.6
- Track training details such as distance, duration, pace, perceived intensity, heart rate responses, resistance work.
- Use a scale to quantify wellbeing ratings on fatigue, stress, quality of sleep, muscle soreness, and irritability.
- Identify any causes of stress/dissatisfaction.
- Illness, injury and menstrual cycle for females.7
- Respect the recovery. It is generally recommended that you should have at least one passive rest day each week.8 The rest day can also act as a ‘‘time-out’’ period and prevent athletes from becoming preoccupied with your sport. Such distractions from the daily routine of training may also alleviate boredom and reduce stress.
Sleep is essential for optimal performance and recovery. Poor duration, quality, and timing of sleep can lead to performance decline, slower recovery, and higher risk of injury in athletes.9 It is generally recommended athletes sleep for the amount of time that is required to feel wakeful during the day, which may vary considerably between individuals. Adults need at least 7 hours of sleep for optimal health and even greater durations are recommended for athletes, adolescents, and children.10
- Optimize nutrition and hydration. Sports dietitians stress the importance of carbohydrate, energy and fluid intake for the prevention of glycogen depletion, a negative energy balance (EB) and dehydration.11,12 Maintaining a positive energy balance will help replenish glycogen and keep stress hormones in check.13 Further, increased dietary protein (3 g/kg/day) intake during a period of overload training in endurance athletes has been shown to decrease performance decline and symptoms of stress.14
Treatment
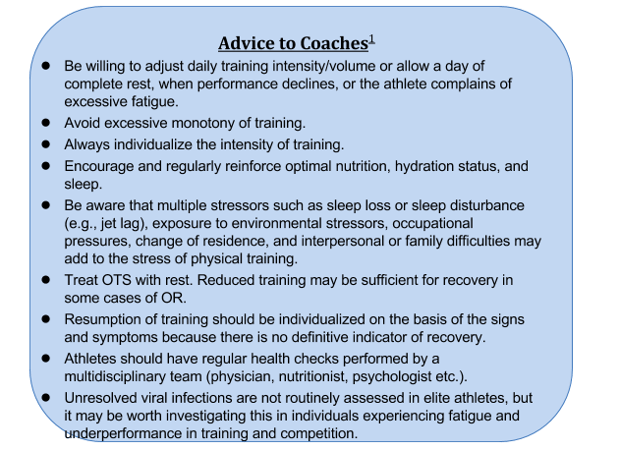
The best treatment of OTS is prevention, mostly by appropriate periodization of the training program with careful focus on including, and executing, appropriate recovery time into the training program. If you reach the point of OTS, a customized treatment plan Is necessary to successfully recover. Concentration should be on relative or absolute rest. Mild cases may recover after only a few weeks of rest or decreased training load. More severe cases of OTS require longer intervals of rest and may not ever resolve.2
Often, a multidisciplinary team consisting of a sports medicine physician, dietitian, psychologist, coach, athletic trainer, and the parents is indicated to address any potential medical etiologies, optimize nutrition, and address any underlying psychological stressors. If you or one of your athletes continues to have symptoms despite extended rest, he or she should be evaluated by a physician to exclude other causes (ie, infection, anemia, injury).
References
- Meeusen R, Duclos M, Foster C, et al. Prevention, diagnosis, and treatment of the overtraining syndrome: joint consensus statement of the European College of Sport Science and the American College of Sports Medicine. Med. Sci. Sports Exerc. 2013; 45:186Y205 .
- Carfagno DG, Hendrix JC.. Overtraining syndrome in the athlete: current clinical practice. Curr Sports Med Rep. 2014 Jan-Feb;13(1):45-51.
- DiFiori J P, Benjamin H J, Brenner J S, Gregory A, Jayanthi N, Landry G L, Luke A. 2014. Overuse injuries and burnout in youth sports: a position statement from the American Medical Society for Sports Medicine. British Journal of Sports Medicine 48 (4): 287-288.
- Matos NF, Winsley RJ, Williams CA. Prevalence of nonfunctional overreaching/overtraining in young English athletes. Med Sci Sports Exerc 2011;43:1287–94.
- Budgett, R. The overtraining syndrome. British Medical Journal. 1994;309(6952).
- Brukner P, Khan K. Clinical sports medicine, 4th ed. Sydney, Australia: McGraw-Hill, 2012:104-105.
- Hooper SL, Mackinnon LT, Howard A, Gordon RD, Bachmann AW. Markers for monitoring overtraining and recovery. Med Sci Sports Exerc. 1995;27(1):106–12.
- Bruin G, Kuipers H, Keizer HA, Vander Vusse GJ. Adaptation and overtraining in horses subjected to increasing training loads. J Appl Physiol. 1994;76:1908–13.
- Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep 2015;38(6):843–4.
- Malhotra R K. 2017. Sleep, Recovery, and Performance in Sports. Neurologic clinics 35 (3): 547-557.
- Meeusen R, Duclos M, Foster C, et al., European College of Sport Science; American College of Sports Medicine. Prevention, diagnosis, and treatment of the overtraining syndrome: joint consensus statement of the European College of Sport Science and the American College of Sports Medicine. Med Sci Sports Exerc 2013;45:186–205.
- Lewis N A, Collins D, Pedlar C R, Rogers J P. 2015. Can clinicians and scientists explain and prevent unexplained underperformance syndrome in elite athletes: an interdisciplinary perspective and 2016 update. BMJ Open Sport & Exercise Medicine 1 (1): e000063-e000063.
- Achten J, Halson SL, Moseley L, Rayson MP, Casey AC, Jeukendrup AE. Higher dietary carbohydrate content during intensified running training results in better maintenance of performance and mood state. J Appl Physiol. 2004;96:1331–40.
- Witard OC, Jackman SR, Kies AK, et al. Effect of increased dietary protein on tolerance to intensified training. Med Sci Sports Exerc 2011;43:598–607.
Disclaimer: This blog is for informational purposes only. Doctors cannot provide a diagnosis or individual treatment advice via e-mail or online. Please consult your physician about your specific health care concerns.
About the Author

Dr. Emily Kraus is a BridgeAthletic performance team contributor where she focuses on topics that are at the forefront of athletics and medicine. She is the incoming Stanford non-operative sports medicine fellow in Physical Medicine and Rehabilitation. Emily has provided medical coverage for events such as the USATF National Track and Field Championships and is the research coordinator for a multi-center study focused on prevention of stress fractures in division I collegiate runners. Emily has finished six marathons, recently ran (and won) her first 50km trail ultramarathon, and placed 56th female in the 2016 Boston Marathon. Emily is passionate about injury prevention, running biomechanics, and the promotion of health and wellness.
Related Posts

The Best Bench Press Variation You’re...
This post is part of our Coaches Corner series with Taylor Rimmer. Taylor is NSCA-CPT, StrongFirst...

Does Powerlifting Harm Heart Health?
A recent study has discovered that a 12-week supervised strength training program (SSTP) may result...
-1.png)
Barefoot Running: Is It For You? |...
Run Free: Consider Less Cushion
Updated October 2020:
With more athletes looking for ways to...